Abstract
Background
The relative efficacy of different sodium-glucose transporter 2 inhibitors (SGLT2i) on cardiorenal outcomes is unclear.
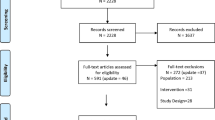
Methods
We included cardiovascular outcome trials (CVOTs) of SGLT2i. The eight endpoints of interest were major adverse cardiovascular events (MACE), myocardial infarction (MI), stroke, cardiovascular death (CVD), CVD or hospitalization for heart failure (HHF), HHF, kidney function progression (KFP), and all-cause death (ACD). We conducted a Bayesian network meta-analysis and calculated the surface under the cumulative ranking curve (SUCRA) probability to rank treatments.
Results
We included ten CVOTs involving five SGLT2i. Canagliflozin (hazard ratio [HR] 0.64; 95% confidence interval [CI] 0.53–0.77), dapagliflozin (HR 0.70; 95% CI 0.62–0.79), empagliflozin (HR 0.68; 95% CI 0.59–0.78), ertugliflozin (HR 0.70; 95% CI 0.54–0.90), and sotagliflozin (HR 0.66; 95% CI 0.56–0.77) versus placebo reduced HHF, whereas none reduced MI and stroke. Empagliflozin reduced CVD or HHF (HR 0.81; 95% CI 0.67–0.99) and KFP (HR 0.65; 95% CI 0.45–0.93), and dapagliflozin reduced KFP (HR 0.69; 95% CI 0.52–0.92), versus ertugliflozin. Canagliflozin had the greatest SUCRA values for the reduction of MACE, stroke, and HHF, whereas empagliflozin had the greatest SUCRA values for the reduction of MI, CVD, CVD or HHF, KFP, and ACD.
Conclusions
Canagliflozin, dapagliflozin, empagliflozin, ertugliflozin, and sotagliflozin versus placebo reduce HHF but none reduces MI and stroke. Canagliflozin is most effective in reducing MACE and HHF, and empagliflozin is most effective in reducing CVD, CVD or HHF, KFP, and ACD. These findings will guide the use of specific SGLT2i in the prevention of different cardiorenal events.









Similar content being viewed by others
References
Bhatt DL, Szarek M, Pitt B, et al. Sotagliflozin in Patients with Diabetes and Chronic Kidney Disease. N Engl J Med. 2021;384:129–39.
Bhatt DL, Szarek M, Steg PG, et al. Sotagliflozin in Patients with Diabetes and Recent Worsening Heart Failure. N Engl J Med. 2021;384:117–28.
Heerspink H, Stefánsson BV, Correa-Rotter R, et al. Dapagliflozin in Patients with Chronic Kidney Disease. N Engl J Med. 2020;383:1436–46.
Packer M, Anker SD, Butler J, et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N Engl J Med. 2020;383:1413–24.
Mcmurray J, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381:1995–2008.
Cannon CP, Pratley R, Dagogo-Jack S, et al. Cardiovascular Outcomes with Ertugliflozin in Type 2 Diabetes. N Engl J Med. 2020;383:1425–35.
Perkovic V, Jardine MJ, Neal B, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380:2295–306.
Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380:347–57.
Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377:644–57.
Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117–28.
Täger T, Atar D, Agewall S, et al. Comparative efficacy of sodium-glucose cotransporter-2 inhibitors (SGLT2i) for cardiovascular outcomes in type 2 diabetes: a systematic review and network meta-analysis of randomised controlled trials. Heart Fail Rev. 2020. https://doi.org/10.1007/s10741-020-09954-8.
Wei XB, Wei W, Ding LL, et al. Comparison of the effects of 10 GLP-1 RA and SGLT2 inhibitor interventions on cardiovascular, mortality, and kidney outcomes in type 2 diabetes: A network meta-analysis of large randomized trials. Prim Care Diabetes. 2021;15:208–11.
Qiu M, Ding LL, Wei XB, et al. Comparative efficacy of glucagon-like peptide 1 receptor agonists and sodium glucose cotransporter 2 inhibitors for prevention of major adverse cardiovascular events in Type 2 diabetes: a network meta-analysis. J Cardiovasc Pharmacol. 2021;77:34–7.
Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–84.
Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Fei Y, Tsoi MF, Cheung B. Cardiovascular outcomes in trials of new antidiabetic drug classes: a network meta-analysis. Cardiovasc Diabetol. 2019;18:112.
Hussein H, Zaccardi F, Khunti K, et al. Cardiovascular efficacy and safety of sodium-glucose co-transporter-2 inhibitors and glucagon-like peptide-1 receptor agonists: a systematic review and network meta-analysis. Diabet Med. 2019;36:444–52.
Alfayez OM, Al YM, Alshibani M, et al. Network meta-analysis of nine large cardiovascular outcome trials of new antidiabetic drugs. Prim Care Diabetes. 2019;13:204–11.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This work was supported by the Shenzhen Key Medical Discipline Construction Fund (SZXK063).
Conflict of interest
Mei Qiu, Liang-Liang Ding, and Hai-Rong Zhou have no potential conflicts of interest that might be relevant to the contents of this manuscript.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent to publication
Not applicable.
Availability of Data and Material
All the original data supporting the findings of this study are available in the supplementary appendixes of this paper.
Code availability
The codes used for the data analyses in this study are available from the corresponding author on reasonable request.
Author contributions
Conception and design: MQ. Administrative support: H-RZ. Provision of study materials or patients: MQ, L-LD, and H-RZ. Collection and assembly of data: MQ, L-LD, and H-RZ. Data analysis and interpretation: L-LD, and MQ. Manuscript writing: MQ, L-LD, and H-RZ. Final approval of manuscript: MQ, L-LD, and H-RZ.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Qiu, M., Ding, LL. & Zhou, HR. Comparative Efficacy of Five SGLT2i on Cardiorenal Events: A Network Meta-analysis Based on Ten CVOTs. Am J Cardiovasc Drugs 22, 69–81 (2022). https://doi.org/10.1007/s40256-021-00484-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-021-00484-8